



Introduction
Burning feet at night is a distressing symptom that can drastically interrupt sleep quality, diminish overall well-being, and signal underlying medical conditions. Millions worldwide experience nighttime foot burning-a phenomenon described as a mix of tingling, numbness, stinging, and heat in the soles-which may worsen wiht rest or inactivity. According to the Mayo Clinic, burning feet (grierson-Gopalan Syndrome or neuropathic paresthesia) can occur in any age group but is especially prevalent in adults over 50 and those with chronic diseases. Understanding its mechanisms and effective, evidence-based approaches-including natural remedies-is vital for sufferers and healthcare providers alike.This thorough guide explores causes, risk factors, clinical evaluation, and holistic strategies to quiet burning feet at night.
Epidemiology: How common is Burning Feet at Night?
Burning sensations in the feet, especially nocturnally, are not rare. Epidemiological studies indicate that up to 10-15% of adults may experience chronic peripheral neuropathy-like symptoms at some point, with diabetes and vitamin deficiencies being major contributors (CDC). The symptom is slightly more prevalent in women and tends to increase with age and comorbidities such as metabolic syndrome, autoimmune diseases, and renal insufficiency (NIH).
Symptomatology: Recognizing Burning Feet at Night
Burning feet at night typically manifests as persistent warmth, stinging, prickling, or pins-and-needles sensations localized to the soles, toes, and sometimes the calves. Notable features include:
- Intensity increases when lying down or at rest
- Symptoms may be accompanied by numbness or tingling (Mayo Clinic)
- Sometimes presents with swelling, redness, or even muscle cramps
- Temporary relief may occur with cooling (e.g., cold floor, water immersion)
Understanding these characteristics helps clinicians and patients differentiate burning feet from other conditions such as plantar fasciitis, restless legs syndrome, or Raynaud’s phenomenon.
Pathophysiology: Why Do Feet Burn at Night?
The burning sensation is often a result of peripheral nerve dysfunction.At night, decreased distractions and reduced external stimuli make neuropathic sensations more apparent. Poor blood circulation, nerve inflammation, or damage impairs normal sensory processing, amplifying uncomfortable thermal and pain signals (NIH). Moreover, hormonal fluctuations, reduced skin moisture, and lower nighttime blood pressure may exacerbate symptoms.
What Causes Burning Feet at Night?
Numerous medical, neurological, metabolic, and environmental factors contribute to nighttime burning feet. Below is a detailed breakdown:
1.peripheral Neuropathy
The leading cause, especially in adults, is peripheral neuropathy-a disorder of the peripheral nerves. Diabetic neuropathy accounts for the majority of cases (CDC), resulting from chronically elevated blood glucose levels that damage nerves and small blood vessels. Other neuropathic causes include:
- Alcohol use disorder
- Vitamin B12 deficiency (Medical News Today)
- Chronic kidney disease (uremic neuropathy)
- Autoimmune disorders (e.g., lupus, Sjögren’s)
- Hereditary neuropathies (Charcot-Marie-Tooth disease)
- HIV-associated neuropathy
2. Diabetes Mellitus
Diabetes is the most prominent risk factor for burning feet worldwide. Diabetic peripheral neuropathy typically presents with burning, tingling, and numbness in a “stocking” distribution, with symptoms worsening at night (NIDDK). The exact mechanisms include oxidative stress, inflammation, and microvascular damage that impair nerve function.
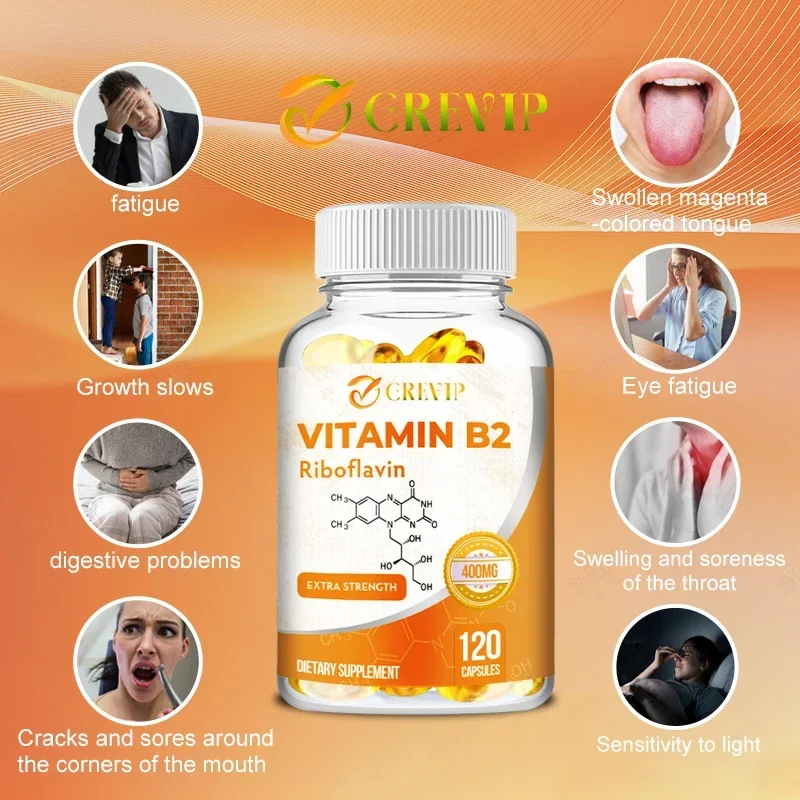
3.Nutritional Deficiencies
Deficiencies in B vitamins (B1, B6, B12), folate, or vitamin E may contribute to nerve degeneration and neuropathic discomfort. Malnutrition, gastrointestinal disorders, and poorly balanced vegetarian or vegan diets increase risk (Harvard Health).
4. Alcohol Use
Excessive alcohol intake is neurotoxic and causes both direct nerve injury and indirect effects via malnutrition (NIH). Alcoholic neuropathy can present as burning, tingling, and muscle weakness, most commonly in the lower limbs.
5. Infectious Diseases
Certain infections-such as HIV, Lyme disease, and hepatitis C-are associated with neuropathy and burning feet symptoms (CDC). Infectious neuropathy may begin with mild paresthesia and proceed to severe burning pain, frequently enough at night.
6. Tarsal Tunnel Syndrome
Compression of the tibial nerve as it passes through the tarsal tunnel (anatomical channel above the ankle) can produce unilateral or bilateral burning, tingling, and weakness of the feet, worse during rest or nocturnal hours (Healthline).
7. Small Fiber Neuropathy
This specific neuropathy affects the small “C” fibers responsible for temperature and pain sensation. Symptoms include burning, stinging, and hypersensitivity, usually exaggerated at night (NIH).
8. Hormonal and endocrine Disorders
Disorders like hypothyroidism, hypothalamic-pituitary axis dysfunction, and menopause (due to hot flashes and vasomotor instability) can elicit burning sensations in extremities, including feet (Mayo Clinic).
9.Medication Side Effects
Drugs known to trigger peripheral neuropathy and burning feet symptoms include some chemotherapies, antihypertensives, anti-retrovirals, and statins. Chemotherapy-induced neuropathy manifests with burning and numbness, commonly during periods of inactivity (National Cancer Institute).
10. Footwear and Environmental Causes
tight shoes, synthetic socks, poor hygiene, and exposure to irritants or allergens can cause contact dermatitis or exacerbate neuropathic discomfort. Prolonged standing and localized pressure on the feet also contribute (NIH).
11. Idiopathic Cases
For some, the etiology remains unidentified despite comprehensive workup; these are termed idiopathic burning feet syndrome (NIH). Age, minor vessel disease, or small fiber dysfunction may play roles.
Clinical Evaluation: When to Seek Medical Attention?
While many causes are benign or reversible, certain warning signs require urgent medical evaluation:
- Progressive or sudden loss of sensation, muscle weakness, or foot drop
- Ulcers, open sores, or signs of infection
- Accompanying symptoms like fever, weight loss, or night sweats
- Unexplained or severe pain disrupting daily life (MedlinePlus)
Healthcare providers may order laboratory tests, nerve conduction studies, skin biopsies, or imaging to diagnose the underlying cause and guide therapy.
Conventional Treatments: Medical Management of Burning Feet
primary treatment targets the root cause-be it diabetes, nutritional deficiency, or neuropathy. Common interventions include:
- Glycemic control in diabetic patients
- B vitamin supplementation (per physician advice)
- Topical therapies: lidocaine, capsaicin cream (NIH)
- Oral medications: gabapentin, pregabalin, duloxetine
- Physical therapy and occupational therapy for nerve health
Pharmacological options may help, but many patients seek complementary, natural remedies to further reduce pain or when medication side effects arise.
Natural Approaches: How to Quiet burning Feet at night
A growing body of research supports several natural, non-pharmacological interventions that may lessen the intensity of nocturnal burning feet. These strategies, grounded in scientific and clinical evidence, include:
1. Cold Water Soaks and Compresses
Immersing the feet in cool (not ice-cold) water for 15-20 minutes may provide temporary relief by numbing nerve endings and reducing local inflammation. A systematic review of hydrotherapy found modest benefits for neuropathic pain, but caution is warranted for patients with diabetes or peripheral vascular disease due to risk of injury.
2. Good Sleep Hygiene and Elevation
Optimizing sleep surroundings-cool room, humidity control, and foot elevation with a pillow-can help. Elevating the feet improves venous return and reduces swelling, which may exacerbate burning sensations (Sleep Foundation).
3. Daily Foot Care
Proper foot hygiene-gentle washing, thorough drying (especially between toes), and using natural fiber socks-minimizes irritation and infection risk. Foot massages or gentle stretching before bedtime encourage circulation and nerve health (Medical news Today).
4. Magnesium and Alpha-Lipoic Acid
Supplement caution: Always consult with your doctor before starting new supplements, especially if you have chronic illness or take regular medication.
Several studies demonstrate that magnesium supplementation may lessen neuropathic pain and reduce muscle cramping. Similarly,alpha-lipoic acid is a potent antioxidant shown in randomized trials to improve symptoms of diabetic neuropathy.
5. B-Complex Vitamins
A meta-analysis published in JAMA highlights the benefits of B1 (thiamine), B6 (pyridoxine), and B12 (cobalamin) in the prevention and management of neuropathic symptoms. Deficiency correction under medical supervision may significantly relieve burning feet.
6. Herbal and Topical Remedies
Research into herbal remedies such as capsaicin (from chili pepper) and camphor/mint balms reveal their utility in reducing pain perception by desensitizing local nerve receptors. Topical capsaicin can offer relief but should be used sparingly and with physician guidance.
7. Regular Low-Impact Exercise
Gentle activities such as walking, swimming, yoga, or tai chi enhance circulation, promote nerve repair, and reduce neuropathic pain (Healthline). structured exercise programs have been shown to reduce intensity and frequency of nocturnal symptoms in neuropathy patients.
8. Anti-Inflammatory Diet
Emerging evidence supports the role of nutritional choices in combating oxidative stress and inflammation-key drivers of neuropathic pain. Diets rich in colorful fruits and vegetables, omega-3s, and low-glycemic foods may benefit those with burning feet (Harvard Health).
9. Mind-Body Therapies
Techniques such as meditation, mindfulness, progressive muscle relaxation, and cognitive behavioral therapy (CBT) have been shown to alter pain perception and improve tolerance, offering adjunctive support to physical treatments (NIH).
Lifestyle modifications to Prevent Nighttime Burning Feet
Adopting the following daily habits may aid in symptom prevention and long-term nerve health:
- Avoid tight or ill-fitting shoes and synthetic socks
- Refrain from walking barefoot, especially on rough surfaces
- Limit alcohol consumption
- Manage blood sugar and blood pressure proactively
- Stay well-hydrated and avoid prolonged standing
- Schedule regular foot checks if you have diabetes or neuropathy
Home Remedies to Try-and What to Avoid
| Recommended | Use With Caution | Avoid |
|---|---|---|
| Cool water soaks (not ice) | Essential oils (patch test first) | Self-medication with prescription drugs |
| Natural fiber socks (cotton/bamboo) | Herbal balms (consult doctor for allergies) | Unlicensed electrical devices or snake oil “cures” |
| Gentle stretching and massage | Supplements (under physician guidance) | Walking on hot, cold, or rough surfaces |
Always consult your healthcare provider before beginning new treatments, especially if you have chronic medical conditions or are pregnant.
Frequently Asked Questions (FAQ) about Burning Feet at Night
What underlying conditions should be screened for?
Persistent or severe burning feet warrants assessment for diabetes, thyroid dysfunction, vitamin deficiencies, and nerve disorders. Early diagnosis of these conditions prevents complications (CDC).
Can burning feet at night be prevented?
Proactive lifestyle measures-including healthy diet, exercise, regular foot care, and prompt management of underlying illness-are effective preventative strategies, especially for high-risk groups (Healthline).
When should I see a doctor?
Seek medical attention if burning feet are recurrent, worsen, impair daily function, or are associated with other neurological symptoms like muscle weakness, ulceration, or mobility loss (Medical News Today).
Conclusion: Balancing natural and Medical Approaches
Burning feet at night can have multifactorial origins-from diabetes and vitamin deficiencies to idiopathic small fiber neuropathy-requiring a thorough, individualized approach to diagnosis and care. effective symptom relief frequently enough arises from a combination of conventional medical treatments and judicious, evidence-based natural therapies. Foot health, sleep optimization, and nutritional adequacy play pivotal roles in managing and preventing nocturnal burning sensations. Always consult with a licensed healthcare provider for persistent or severe symptoms, and before starting new supplements or therapies. By addressing both underlying causes and providing symptomatic relief, individuals can greatly improve sleep quality, daily functioning, and overall quality of life.
Resources and Further Reading
- Mayo Clinic: Burning Feet Syndrome – Symptoms & Causes
- NHS: Peripheral Neuropathy Overview
- CDC: Diabetic Neuropathy Facts
- Harvard Health: Diabetic neuropathy and Foot Care
- MedlinePlus: Burning feet



