What Is Leaky Gut Syndrome and How Do You Heal It Naturally?
Introduction
Leaky Gut Syndrome has emerged as a compelling topic in both clinical gastronterology and mainstream health circles. As rates of chronic inflammatory and autoimmune conditions rise globally, researchers and clinicians have noted increasing interest in the gut barrier’s role in overall health. The gastrointestinal tract’s integrity is critical for maintaining immune balance, nutrient absorption, and protection against pathogens. Disruption of this balance, sometimes referred to as “leaky gut,” has been hypothesized to contribute to a wide spectrum of diseases. yet, the medical community remains divided on how to define, assess, and manage this condition, especially using natural approaches. This article examines current medical understanding, underlying mechanisms, clinical implications, and evidence-based natural strategies for improving gut barrier function.
Understanding the gastrointestinal Barrier
The human gut is lined by a single layer of epithelial cells that function as a highly selective barrier. Tight junctions between these epithelial cells regulate the passage of nutrients, electrolytes, and water while restricting the entry of harmful substances, antigens, and microbes. This mucosal barrier works in concert with the gut-associated lymphoid tissue (GALT) and microbiota to prevent systemic inflammation and infection (NIH).
Disruption in gut barrier function-sometimes known medically as increased “intestinal permeability”-can allow bacterial endotoxins, food antigens, and pathogens to translocate into the bloodstream, potentially triggering immune dysregulation. This phenomenon is thought to be a precursor or exacerbating factor for several inflammatory, allergic, and autoimmune diseases.
What Is Leaky Gut Syndrome?
Clinical Definition and Debate
“Leaky Gut Syndrome” is a lay term used to describe a constellation of symptoms allegedly resulting from increased intestinal permeability. Though, in mainstream medicine, the diagnosis is not universally accepted due to insufficient criteria and lack of consensus on causality.Most research and clinical guidelines instead refer to the more precise term, “increased intestinal permeability” (Harvard Health).
Despite the controversy, a growing body of studies links abnormal gut permeability with conditions such as celiac disease, inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), type 1 diabetes, obesity, and certain autoimmune diseases (NIH). This suggests that the gut barrier’s integrity plays a notable role in overall health.
Pathophysiology
Intestinal permeability is regulated primarily by the tight junction proteins (occludin,claudins,and zonulin). When these proteins are disrupted by factors such as infections,stress,poor diet,excessive alcohol,nonsteroidal anti-inflammatory drugs (NSAIDs),or bacterial overgrowth,the mucosal barrier can become compromised. This may lead to the unwanted translocation of immune-reactive substances into the circulation, precipitating local and systemic inflammatory responses (NIH).
Symptoms and Clinical Manifestations
The proposed symptoms associated with leaky gut are diverse and often overlap with other health issues. They may include:
- Chronic diarrhea, constipation, or bloating
- Abdominal pain
- Food sensitivities or intolerances
- Fatigue
- brain fog or cognitive difficulty
- Joint pain
- Unexplained skin rashes or conditions such as eczema
- Autoimmune flare-ups
- mood disturbances such as anxiety or depression
It is essential to note that such symptoms are nonspecific and may indicate various underlying conditions. Definitive diagnosis of increased intestinal permeability often requires specialized tests, such as the lactulose-mannitol test or serum zonulin levels (NIH).
Underlying causes and Risk Factors
Several modifiable and non-modifiable factors contribute to impaired gut barrier function:
| Factor | Mechanism | Evidence |
|---|---|---|
| Diet high in processed foods and sugar | Promotes gut dysbiosis and inflammation | NIH |
| Chronic stress | Alters gut motility and cytokine production | NIH |
| Excess alcohol consumption | Damages mucosal lining,increases permeability | NIH |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Disrupt tight junction proteins | NIH |
| Infections (bacterial, viral, fungal) | Damage epithelial cells, induce immune dysregulation | NIH |
| Gut dysbiosis | Disrupts microbial balance, affects barrier integrity | NIH |
| Autoimmune disease | Triggers immune-mediated epithelial damage | NIH |
Medical Controversy Around Leaky Gut
While increased intestinal permeability is a well-recognized phenomenon in certain diseases (e.g., celiac disease, Crohn’s disease), the concept of “Leaky Gut Syndrome” as an autonomous clinical diagnosis remains unproven.Major health organizations such as the NHS and Mayo Clinic caution against definitive claims,emphasizing the necessity for more research.
Nonetheless, there is widespread agreement on the importance of maintaining gut barrier function, particularly for individuals with risk factors or co-occurring gastrointestinal and immune-related conditions.
How Is Increased Intestinal Permeability Diagnosed?
Traditional diagnosis focuses on ruling out underlying conditions through clinical evaluation and laboratory testing. Objective assessment of gut permeability may include:
- Lactulose-Mannitol Test: Measures urinary excretion of two non-metabolizable sugars following oral ingestion (NIH).
- Serum Zonulin Levels: Biomarker for tight junction dysfunction (NIH).
- Endoscopic or Histological Evaluation: In cases of suspected autoimmune enteropathies.
However, none of these tests are routinely recommended in the absence of clinically significant symptoms or underlying pathology.
The Gut Microbiome and Barrier Function
The gut microbiome comprises trillions of bacteria that influence gut barrier integrity, immune function, and nutrient synthesis. An imbalance in microbial populations (dysbiosis) is associated with increased intestinal permeability and systemic inflammation (Nature).
Certain commensal species, such as Lactobacillus and Bifidobacterium, help reinforce the mucosal barrier and out-compete pathogenic bacteria. Microbial metabolites, especially short-chain fatty acids (SCFAs) like butyrate, are essential for nourishing colonocytes and maintaining tight junction integrity (NIH).
Conditions Associated with Increased Intestinal Permeability
- Celiac Disease: Gluten intake in genetically susceptible individuals activates zonulin, increasing gut permeability (NIH).
- Crohn’s Disease and ulcerative Colitis: Chronic inflammation disrupts tight junctions (NIH).
- irritable Bowel Syndrome: Low-grade barrier dysfunction reported in some subtypes (NIH).
- Type 1 Diabetes: Leaky gut may precede autoimmune pancreatic beta cell destruction (NIH).
- Obesity and Metabolic Syndrome: Increased gut permeability may contribute to systemic inflammation and insulin resistance (NIH).
Can Leaky Gut Be healed Naturally?
Many clinicians advocate for a holistic, individualized approach to optimizing gut health, incorporating nutrition, lifestyle modification, and-when appropriate-evidence-based supplements or probiotics. Below,natural interventions are reviewed according to the available clinical data.
Dietary Interventions
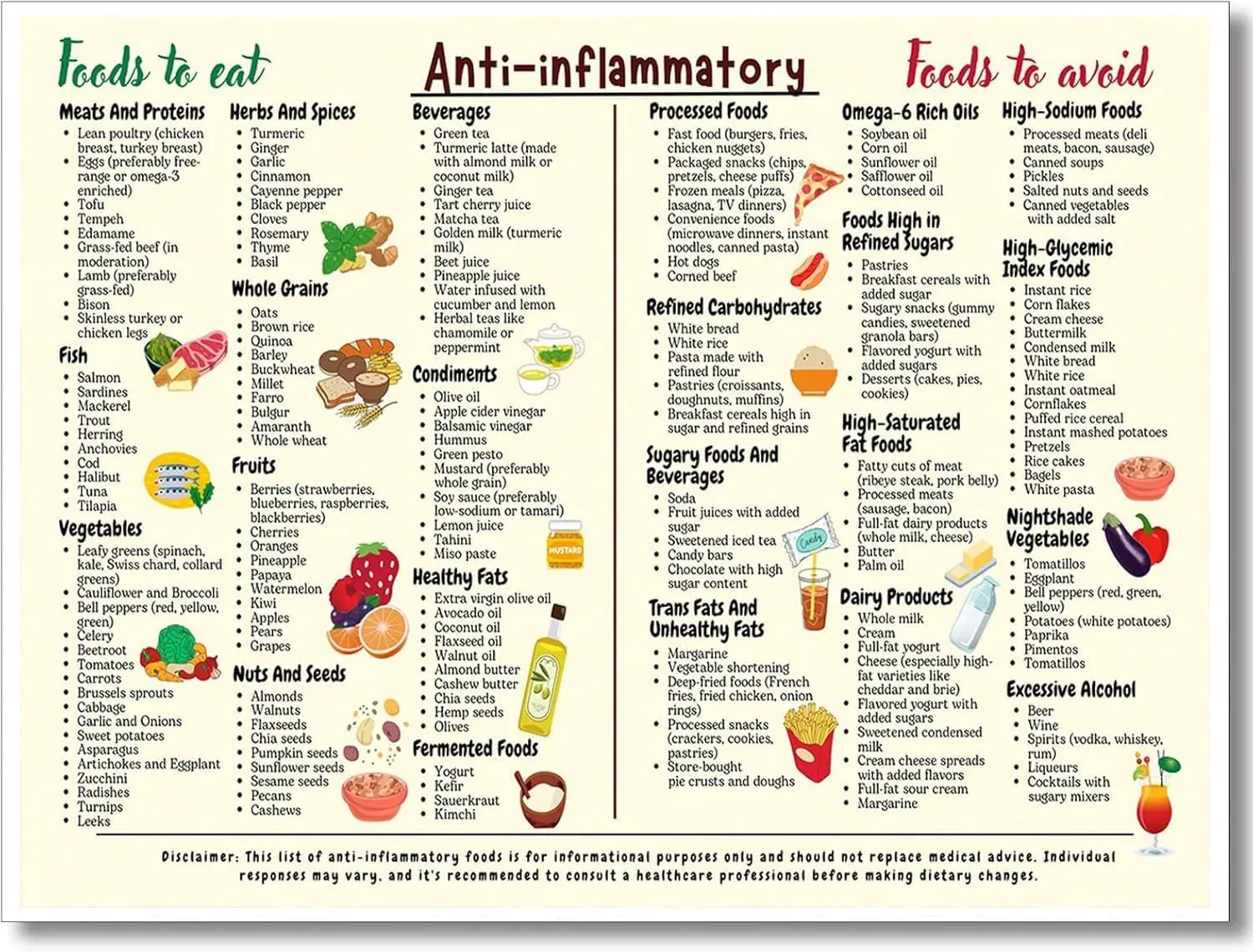
1. Anti-inflammatory Whole Foods Diet
Consuming a multitude of fiber-rich fruits, vegetables, legumes, nuts, seeds, whole grains, and omega-3-rich fatty fish may reduce intestinal inflammation and promote microbial diversity (Harvard Health).
- Polyphenols (berries,cocoa,olives) have prebiotic effects and can modulate tight junctions (NIH).
- Soluble fiber (oats, legumes) is fermented by gut bacteria producing SCFAs, which enhance epithelial health (NIH).
2.Elimination of Trigger Foods
For sensitive individuals, temporary elimination of gluten, dairy, eggs, or other potential antigens might potentially be warranted under medical supervision.This approach has shown benefits for certain patients with irritable bowel syndromes, food sensitivities, or autoimmune disease flare-ups (NIH).
3. Limiting Processed and Ultra-Processed Foods
Diets high in emulsifiers, additives, refined sugars, and saturated fats can disrupt gut microbiota composition and increase permeability (NIH).
Probiotics and Fermented Foods
Probiotics-live microbes conferring health benefits-may repair gut barrier function by modulating inflammation, pathogen competition, and synthesizing SCFAs (NIH). Specific strains such as lactobacillus rhamnosus or Bifidobacterium animalis have demonstrated positive effects in clinical trials.
- Yogurt, kefir, sauerkraut, kimchi, kombucha, and miso provide a range of beneficial microbes.
- Probiotic supplementation may support intestinal health,but optimal strain and dosage vary between individuals and conditions (Healthline).
Prebiotics and Dietary Fiber
Prebiotics are non-digestible food components that stimulate the growth of beneficial bacteria. Common prebiotics include inulin, fructooligosaccharides, and resistant starch found in foods like garlic, onions, bananas, asparagus, and legumes (NIH).
Increasing prebiotic intake can enhance microbial diversity and butyrate production, which is vital for tight junction integrity and anti-inflammatory effects (NIH).
Lifestyle Modifications to Support Gut Health
Stress Reduction
Psychological stress adversely impacts gut motility, microbiota composition, and permeability via the hypothalamic-pituitary-adrenal (HPA) axis. Mind-body interventions such as mindfulness meditation, cognitive behavioral therapy, yoga, and adequate sleep have been shown to improve gut symptoms in IBS and other conditions (NIH).
Regular Physical Activity
Moderate, consistent exercise enhances microbial diversity, reduces gut inflammation, and strengthens the epithelial barrier (NIH).
Adequate Sleep
Chronic sleep deprivation may exacerbate gut inflammation and increase permeability. Prioritizing restorative sleep (7-9 hours/night) is recommended for optimal immune and gut function (NIH).
Evidence-based Nutritional and Herbal Supplements
Certain nutrients and herbal remedies have been studied for their role in restoring barrier integrity:
- Glutamine: Promotes enterocyte regeneration and tight junction protein expression. Particularly helpful after gastrointestinal infections or in athletes (NIH).
- Curcumin (turmeric extract): Potent anti-inflammatory and antioxidant effects (NIH).
- Zinc carnosine: Supports mucosal healing and has shown benefit in peptic ulcer and IBD patients (NIH).
- Aloe vera extract: May reduce inflammation and promote repair in mild IBD (NIH).
- omega-3 fatty acids: Anti-inflammatory effects, found in fatty fish and algal oil supplements (NIH).
supplement use should be guided by a licensed healthcare provider, particularly for individuals on chronic medications or with complex medical histories.
When to Seek Medical Advice
It is crucial to consult a healthcare professional if you experience persistent gastrointestinal symptoms such as unexplained weight loss, blood in stool, intractable diarrhea, or severe abdominal pain.These may indicate underlying conditions such as IBD, celiac disease, or infections that require targeted medical therapy (Mayo Clinic).
Self-diagnosis or unsupervised elimination diets without medical direction may lead to nutritional deficiencies.
Summary: Integrating Natural Strategies Safely
Leaky gut Syndrome-more precisely, increased intestinal permeability-remains an evolving field in gastroenterology and immunology. While definitive diagnostic and therapeutic guidelines are lacking, maintaining gut barrier integrity is crucial for both digestive and extra-digestive health. An evidence-based, natural approach involves:
- Diversifying the diet with fiber-rich, anti-inflammatory foods
- Incorporating probiotic and prebiotic foods
- reducing intake of processed foods, added sugars, excess alcohol, and NSAIDs when possible
- Managing stress and optimizing sleep and exercise
- Consulting a professional regarding the use of carefully selected supplements
More robust clinical research is needed to clarify the role of natural interventions and to identify which patients are most likely to benefit. Until then, a holistic, individualized approach-guided by current science and a qualified healthcare provider-remains the safest strategy for gut health.
Frequently Asked Questions (FAQs)
Is Leaky Gut Syndrome recognized by mainstream medicine?
While “leaky gut” is not a formal diagnosis, increased intestinal permeability is established in several diseases and remains an active area of research (Medical News Today).
Can diet alone cure leaky gut?
diet can help restore gut barrier integrity, but results may vary depending on underlying health conditions. A combination approach is advised (Healthline).
What foods should I avoid?
Ultra-processed foods, refined sugars, excess alcohol, and food antigens (for sensitive individuals) may exacerbate permeability. Always tailor restrictions with medical oversight.
Are probiotics beneficial?
Clinical studies support probiotic use in select groups, particularly those with IBS or antibiotic-induced dysbiosis (NIH).
Do supplements work?
Supplements such as glutamine, zinc carnosine, and omega-3 fatty acids show promise but should only be taken after professional evaluation.
References
- Harvard Health – The Truth About Leaky Gut
- National Library of Medicine – PubMed
- NIH – PubMed Central
- Mayo Clinic Q&A: Leaky Gut Syndrome
- NHS – leaky Gut Syndrome
- medical News Today – What Is Leaky Gut?
- Centers for Disease Control and Prevention
Conclusion
Awareness of gut barrier function and related lifestyle strategies is increasing in relevance as evidence connects digestive and systemic health. Anyone experiencing persistent or severe digestive symptoms should seek expert evaluation to exclude serious underlying conditions. For those seeking to optimize gut health naturally, an individualized approach-grounded in medical science and supported by an integrative practitioner-offers the best path forward.