Introduction
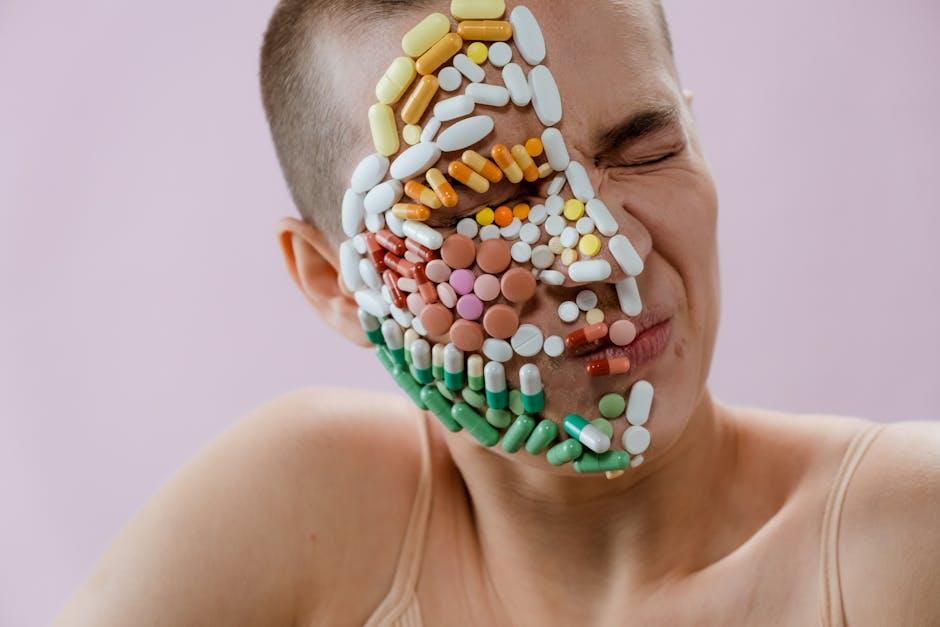
Vitamin A is a fat-soluble micronutrient essential for vision, immune function, reproduction, and cellular communication. While vitamin A deficiency remains a public health problem in some parts of the world, notably among children and pregnant women, increasing awareness of the importance of micronutrients has led some individuals—often in high-income countries—to overconsume vitamin supplements, inadvertently risking toxicity. According to the World Health Organization (WHO), vitamin A supplementation programs have saved countless lives, yet the problem of hypervitaminosis A—chronic or acute vitamin A overdose—remains under-recognized, with both immediate and subtle health consequences.
This article provides an evidence-based overview of the signs and symptoms of vitamin A overdose, underlining key risk factors, clinical ramifications, diagnosis, and prevention strategies. it draws upon current recommendations from leading health institutions, ensuring you get medically accurate and actionable details.
Understanding Vitamin A: Basic Physiology & Sources
What is Vitamin A?
Vitamin A is a group of organic compounds—including retinol, retinal, retinoic acid, and several provitamin A carotenoids such as beta-carotene—that are vital for numerous physiological processes. The human body obtains vitamin A through two main forms:
- Preformed vitamin A (retinol and retinyl esters): Found in animal sources such as liver, fish oils, milk, and eggs.
- provitamin A carotenoids: plant-derived compounds (e.g.,beta-carotene) that convert into retinol within the body. Common sources include carrots, sweet potatoes, and spinach (NIH Office of Dietary Supplements).
The Role of vitamin A in Human Health
Vitamin A supports several critical functions:
- Vision: Constituent of rhodopsin, which enables scotopic (low-light) vision.
- Immunity: Modulates immune defense by supporting mucosal barriers and lymphocyte function (NCBI PMC).
- cell Growth and Differentiation: Required for normal cell development and epithelial integrity.
- Reproduction: Supports sperm development, fetal growth, and placental health.
Recommended Dietary Allowances
The National Institutes of Health recommends the following daily intake (measured as micrograms of retinol activity equivalents, RAE):
- Men, age 19+: 900 mcg RAE
- Women, age 19+: 700 mcg RAE
- Pregnant women: 770 mcg RAE
- Lactating women: 1,300 mcg RAE
Intakes consistently above these levels—especially from supplements or animal sources—can result in toxicity.
What Constitutes Vitamin A Overdose?
Definitions: Hypervitaminosis A
Vitamin A overdose (hypervitaminosis A) refers to a state where excessive vitamin A accumulates in body tissues, causing clinical manifestations. It can be acute (from a single massive dose) or chronic (from prolonged, excessive intake).
- Acute toxicity typically results from ingestion of very large amounts (frequently enough > 660,000 mcg RAE or >200,000 IU in a short period for an adult).
- Chronic toxicity is more common, usually developing after daily intake exceeding 3,000 mcg RAE (10,000 IU) over several months (Healthline; Mayo Clinic).
Sources of Vitamin A Overdose
- Supplements: Most overdoses are caused by high-dose vitamin A supplements or multivitamins.
- Liver consumption: Regular ingestion of large amounts of animal liver (e.g., polar bear, seal) can cause toxicity.
- Accidental pediatric ingestion: Children consuming flavored vitamin A gummies or concentrates are particularly at risk.
- Medications: Some prescription medications (e.g.,isotretinoin for acne) are vitamin A derivatives and can contribute to overdose.
Who Is Most at Risk?
- Children (especially < five years)
- Pregnant women
- Elderly individuals
- Individuals with chronic illnesses affecting liver function
- Persons misusing vitamin supplements or consuming herbal remedies or fortified foods in excess
Individuals with pre-existing liver disorders or those concurrently taking hepatotoxic drugs may experience more severe effects at lower doses.
Importantly,toxicity is rare from foods naturally rich in beta-carotene,as the conversion to retinol is regulated. However, preformed vitamin A or synthetic retinoids bypass this control.
What Are the Signs and Symptoms of Vitamin A Overdose?
recognizing vitamin A toxicity can be challenging due to variable, frequently enough subtle symptoms, particularly in chronic cases. Many signs overlap with other conditions, complicating diagnosis. Here’s a detailed, evidence-based overview.
1. Dermatologic Signs
- Dry, peeling, or itchy skin: Excess vitamin A disrupts keratinocyte differentiation, resulting in xerosis (abnormally dry skin), desquamation, and increased sensitivity.
- Cracked lips (cheilitis) and mouth ulcers: Mucocutaneous involvement often presents with angular cheilitis.
- Alopecia (hair loss): Follicular hyperkeratosis and hair thinning are reported with chronic overdose (NCBI Bookshelf).
2.Neurological and Musculoskeletal Effects
- Headache and intracranial hypertension: Elevated intracranial pressure (pseudotumor cerebri) manifests as a persistent headache, sometimes with blurred or double vision.
- Bone and joint pain: Excess vitamin A activates osteoclasts, increasing risk of bone pain, arthralgia, and—over time—osteoporosis or spontaneous fractures (Mayo Clinic: Vitamin A and Bone Health).
- Muscle weakness due to altered protein metabolism.
3.Gastrointestinal Manifestations
- Nausea and vomiting: Especially prominent in acute toxicity episodes.
- Loss of appetite and weight loss
- abdominal pain
- Hepatomegaly (enlarged liver): Chronic hypervitaminosis A can lead to hepatic inflammation and fibrosis (early stages of liver damage) (StatPearls, Hepatotoxicity).
4. Visual Disturbances
- Blurred vision and diplopia (double vision): Result from raised intracranial pressure or direct effects on the optic nerve.
- Photophobia (light sensitivity): May occur with papilledema.
5.Generalized Symptoms
- Fatigue and drowsiness
- Irritability, confusion, or mood changes: Reported with both acute and chronic toxicity.
- Fever, malaise: Generalized illness can mimic viral syndromes.
6. Hepatotoxicity and Systemic Effects
- Elevated liver enzymes and bilirubin: Chronic overdose poses a risk of developing hepatitis and cirrhosis.
- Jaundice (yellowing of skin and eyes): Suggests advanced hepatic involvement.
- Portal hypertension in severe,long-standing cases.
7. Specific Signs in Children
- Bulging fontanelles (soft spots) in infants: Due to increased intracranial pressure.
- Failure to thrive: Poor growth, irritability, and vomiting (CDC: Vitamin A Toxicity in Infants).
- Drowsiness and lethargy
8.Teratogenic Effects
Vitamin A is a known teratogen, and excessive intake during pregnancy increases the risk of birth defects affecting the CNS, heart, and craniofacial structure. Pregnant women should not exceed recommended intakes (NHS: Vitamins in Pregnancy).
Pathophysiology of Vitamin A Toxicity
Unlike water-soluble vitamins, vitamin A is stored in the liver and adipose tissues. Chronic excess saturates hepatic stellate cells, resulting in leakage into circulation and deposition in various tissues. Toxic levels interfere with membrane integrity, mitochondrial function, and genetic regulation, accounting for multisystem involvement (NCBI PMC: Vitamin A toxicity).
Bone resorption: retinoic acid stimulates osteoclasts and antagonizes vitamin D, promoting bone fragility and increased fracture risk (JAMA: Vitamin A and Bone Health).
Hepatotoxicity: Hepatic stellate cell activation leads to fibrosis, reduced synthetic function, and ultimately cirrhosis with long-term exposure.
Neurological dysfunction: High serum retinol can cause cerebral edema and increased pressure in cerebrospinal fluid.
Diagnosis: How Is Vitamin A Toxicity Identified?
Given the nonspecific symptoms, clinicians must maintain a high index of suspicion, especially in patients with a history of supplement use or unusual diets.
Clinical Assessment
- Thorough history: Supplement intake, diet, known liver disorders, medication history (notably retinoids).
- Physical examination: Focus on dermatologic, neurological, and hepatic signs.
Laboratory Testing
- Serum retinol measurement: Levels >2.5 micromol/L (70 mcg/dL) are suggestive, but can fluctuate.
- Liver function tests: Elevated AST, ALT, bilirubin as evidence of hepatic damage.
- Imaging: in advanced cases, liver ultrasound or bone scans might potentially be indicated.
It’s significant to note that serum retinol levels do not always correlate with toxicity, and clinical context is critical for interpretation (MedlinePlus).
Potential Complications & Prognosis
- Liver disease: Chronic intake may cause irreversible fibrosis or cirrhosis, especially in predisposed individuals.
- Chronic bone demineralization: Risk of spontaneous fractures, especially in the elderly.
- Severe neurological symptoms: Papilledema may result in vision loss if untreated.
- Teratogenicity: birth defects if excess occurs during critical periods of pregnancy.
In children, acute encephalopathy or liver failure may occur and can be life-threatening.
With early diagnosis and withdrawal of excess vitamin A, most patients recover without permanent sequelae; though, advanced liver or bone complications might potentially be irreversible.
How Much Is Too Much? Safe Upper Limits Explained
The NIH defines the Tolerable Upper Intake Level (UL) of vitamin A as:
| Age Group | UL (mcg RAE/day) | UL (IU/day) |
|---|---|---|
| Children (1–3 years) | 600 | 2,000 |
| Children (4–8 years) | 900 | 3,000 |
| Children (9–13 years) | 1,700 | 5,667 |
| Teens (14–18 years) | 2,800 | 9,333 |
| Adults (19+ years) | 3,000 | 10,000 |
Intakes above these thresholds—especially daily, for months—can result in chronic toxicity.Beta-carotene supplements have a different risk profile but should not be consumed excessively, especially by smokers, due to associations with lung cancer (PubMed).
Prevention and Best Practices
- Avoid needless supplements: Unless prescribed for deficiency, most adults with balanced diets do not need high-dose vitamin A pills.
- Read supplement labels: Carefully check the form and dosage of vitamin A; dosages are often listed as IU or mcg RAE—be aware of conversions (FDA Nutrition Label Guide).
- Limit liver intake: Occasional liver in a normal diet is safe, but daily consumption or “superfood” extremes increase risk.
- Pregnant women: Use only prenatal vitamins meeting current safety guidelines for vitamin A.
- Inform your physician: Always disclose supplement use, especially if you develop unexplained health changes.
What To Do If You Suspect Overdose
- discontinue supplements or high-vitamin A foods immediately.
- Consult a healthcare provider promptly: Early intervention prevents complications.
- Report concerning symptoms: Severe headache, blurred vision, yellow skin, or unexplained fatigue warrant medical attention.
- In acute overdose, especially with children, seek urgent care. Activated charcoal and gastric decontamination may be required (Mayo clinic First aid).
Frequently Asked Questions (FAQ)
- Can you get vitamin A toxicity from food?
Only by consuming very high amounts of animal liver or taking certain animal-based supplements. Plant-based (beta-carotene) foods do not cause toxicity as their conversion to retinol is regulated (Harvard Health).
- Are multivitamins perilous?
Most commercial multivitamins are safe when used as directed. Dangers arise from “megadose” supplements, improper use, or overlapping products containing vitamin A.
- Does vitamin A toxicity cause orange skin?
- No: Orange skin (carotenemia) results from excessive beta-carotene—not retinol—consumption. It is indeed benign and not toxic, mostly seen in infants and children who eat large amounts of carrots or sweet potatoes.
- Is vitamin A toxicity reversible?
In most early and moderate cases, yes. Prolonged, severe exposure may cause permanent hepatic or skeletal damage.
Conclusion
While vitamin A is indispensable for health, “more” is not better. Both acute and chronic overdoses are associated with a spectrum of dermatologic, neurological, hepatic, and systemic complications that can be serious—particularly in children and those with underlying comorbidities. Through a balanced diet and judicious supplement use, the risk of hypervitaminosis A is fully preventable. If you suspect overdose or experience unexplained health symptoms with supplement use, seek evaluation from your healthcare provider for prompt diagnosis and treatment.
for more authoritative information on vitamin A, refer to these comprehensive resources:

