lower back pain“>
lower back pain“>
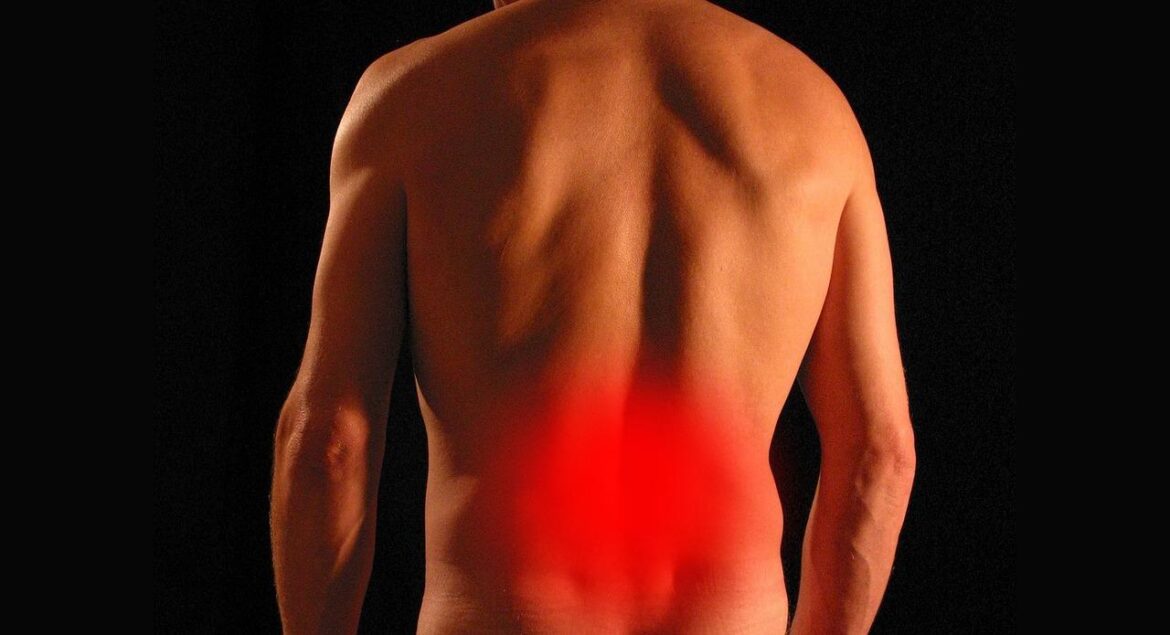
Lower back pain during simple movements you did not expect
Introduction
Lower back pain is a leading contributor to global disability,affecting individuals of all ages and backgrounds. According to the World Health Organization (WHO), low back pain affects an estimated 619 million people worldwide, making it the single most common musculoskeletal cause of disability. Notably, lower back pain during simple, seemingly innocuous movements—like reaching for a light object, tying shoelaces, or standing up—can be alarming and interfere profoundly with daily functioning. Understanding why lower back pain occurs during simple movements you did not expect is essential for prevention,effective management,and improved quality of life.This article provides a comprehensive, evidence-based exploration of the causes, symptoms, diagnosis, prevention, and treatment of lower back pain triggered by unexpected simple movements.
Overview and Definition
Lower back pain (LBP) is clinically defined as pain localized between the lower margin of the twelfth rib and the lower gluteal folds, frequently accompanied by restricted mobility and potential referral pain to the legs. In medical practice,lower back pain is further classified as acute (pain lasting less then 6 weeks),subacute (6–12 weeks),or chronic (greater than 12 weeks) [PubMed]. LBP can result from various underlying pathologies, including musculoskeletal strain, intervertebral disc disorders, facet joint dysfunction, and nerve root irritation. According to the National Institutes of Health (NIH), around 80% of adults will experience low back pain at some point in their lives, underscoring the staggering prevalence of this condition.
The lumbar region, comprising the five vertebrae labeled L1 through L5, is notably susceptible due to its role in bearing most of the body’s weight and facilitating movement. while heavy lifting or trauma are commonly recognized triggers, a significant proportion of cases develop in the absence of major exertion—sometimes during simple daily motions that would not typically be considered risky.
Causes and Risk Factors
Understanding why sudden lower back pain occurs during movements as simple as bending, standing, or twisting requires an in-depth exploration of musculoskeletal, neurological, and lifestyle factors. These causes and risk factors can often act synergistically.
Muscle Strain and Ligament Sprain
One of the most prevalent causes of acute lower back pain during unexpected movements is muscle or ligament strain [Mayo Clinic]. Even subtle flexion or twisting can overextend or micro-tear the soft tissues of the lower back, especially if the muscles are fatigued or the ligamentous support is compromised. These micro-injuries trigger a localized inflammatory response, resulting in pain, stiffness, and sometimes muscle spasms.
Intervertebral Disc Pathology
Degeneration or herniation of the intervertebral discs—fibrocartilaginous cushions between the vertebrae—can impinge on spinal nerves. Everyday actions such as sitting down or picking up a pencil can provoke sharp pain if a compromised disc shifts or presses against neural tissue [NHS].
Facet Joint Dysfunction
Facet joints,small stabilizing joints at each vertebral segment,can develop arthritic or degenerative changes over time. Simple motions, particularly twisting or arching the back, can provoke pain if these joints become misaligned or inflamed [Harvard Health].
Poor Core Stability and muscle Imbalance
Insufficient strength and coordination in core muscles predispose to lower back vulnerability during trivial movements.Weak or uncoordinated abdominal and paraspinal muscles force the lumbar region to absorb stresses inefficiently, increasing the likelihood of injury [Healthline].
Degenerative Spine Disease
Aging is associated with wear-and-tear changes, including osteoarthritis, spondylosis, and spinal stenosis. Such conditions narrow the spinal canal or joint spaces, causing nerves to become pinched during even gentle movement [MedlinePlus].
ural Stress and Ergonomics
Frequent poor ure or ergonomically unsound work environments can lead to chronic, low-grade overload of the lumbar structures. Over time,this makes the lower back susceptible to sudden pain even when stress levels are low [CDC].
Other Medical Conditions
Other contributors include vertebral compression fractures (especially in osteoporosis), inflammatory conditions like ankylosing spondylitis, infections, or rarely, malignancies [Mayo Clinic].
Risk Factor Summary
- Advanced age
- Obesity
- Sedentary lifestyle
- Poor physical conditioning
- Occupational hazards or repetitive movements
- Previous back injury
- Poor lifting technique
- Smoking (impairs blood flow to discs)
- Chronic stress affecting muscle tension and pain perception
Pathophysiology: How Simple Movements Trigger pain
The lumbar spine is a delicate, complex system balancing flexibility and stability. Even everyday movements can trigger pain when underlying vulnerability exists. Here’s how:
- Microtrauma Accumulation: Repetitive overuse, sustained poor ure, or insufficient recovery after minor injuries can lead to cumulative microtrauma. Eventually, an innocuous movement may “tip the scale,” resulting in acute pain [JAMA].
- Nerve Impingement: Disc or osteophyte (bone spur) impingement may not cause symptoms until a movement compresses the nerve root, producing sudden pain, numbness, or tingling [PubMed Central].
- Muscle Guarding and Spasm: Previously strained or weak muscles may react with acute spasm or guarding in response to unexpected stretching or contraction, even during simple actions [Harvard Health].
- Altered Proprioception: With core muscle fatigue or ural abnormalities, the brain’s sense of body position (proprioception) is impaired, increasing the risk of abrupt, uncoordinated movement and injury [PMC].
Epidemiology: Prevalence and Demographics
Epidemiological data from the Centers for Disease Control and Prevention (CDC) indicate that lower back pain is the most common type of job-related disability and the leading cause of missed workdays worldwide. In adults, prevalence increases with age, peaking between ages 40–69, and is slightly more common in females due to differing biomechanics and hormonal influences. Occupational groups with high physical demands or prolonged sitting/standing are particularly at risk [NCBI].
| population | prevalence of Lower Back Pain (%) | Source |
|---|---|---|
| General Adults (worldwide) | ~7.5% at any time | WHO |
| US Adults | ~25% report recent LBP | CDC |
| Workers with physically demanding jobs | Up to 50% | NIOSH |
Clinical Presentation and Symptomatology
Lower back pain during simple, unanticipated movements typically presents with:
- Sudden onset of sharp, stabbing, or pulling pain localized in the lumbar region
- Muscle tightness, stiffness, or “locking” sensation
- Pain radiating into the gluteal area or thighs (if nerve roots are affected)
- Difficulty straightening, bending, or resuming activity after pain onset
- Potential numbness, tingling, or weakness (neurological involvement)
- Increased pain with particular positions or further movements (mechanical component)
Severity ranges from mild, transient discomfort to debilitating, immobilizing pain. Intensity does not always correlate with severity of underlying injury.
red Flags: When Lower Back Pain Warrants Urgent Evaluation
While most cases of lower back pain are benign and resolve with conservative care, certain features—known as “red flags”—necessitate prompt medical attention [Mayo Clinic]:
- Sudden severe pain following trauma (e.g.,fall,collision)
- progressive leg weakness or numbness
- Loss of bowel or bladder control (cauda equina syndrome)
- Unexplained weight loss,fever,or chills (possible infection/malignancy)
- History of cancer,osteoporosis,IV drug use,or immunosuppression
Diagnosis: Clinical Assessment and Investigations
Accurate diagnosis begins with a thorough medical history focusing on the onset,quality,duration,and aggravating/relieving factors of pain,as well as occupational and personal risk factors. Physical examination evaluates:
- Palpation for localized tenderness or muscle spasm
- Range of motion testing (flexion, extension, rotation)
- Neurological examination for sensory, motor, and reflex changes
Most acute, non-traumatic lower back pain does not require imaging unless red flags are present or pain persists beyond 4–6 weeks [NCBI]. When indicated, investigations include:
- X-rays: Assess bone structure, fractures, and major degenerative changes.
- MRI or CT scans: Identify herniated discs, spinal stenosis, or soft tissue pathology.
- Laboratory tests: Performed if infection or inflammatory disease is suspected.
Differential Diagnosis
While mechanical causes predominate, a wide range of pathologies must be considered in persistent or atypical cases:
- Vertebral compression fracture (especially in elderly or osteoporotic patients)
- ankylosing spondylitis or other spondyloarthropathies
- Spinal infections (e.g., osteomyelitis, discitis)
- Metastatic malignancy
- Abdominal or pelvic organ referral (aortic aneurysm, pancreatitis, endometriosis, etc.)
Timely identification of non-mechanical lower back pain is critical for guiding appropriate therapy [the Lancet].
Therapeutic Protocols: Acute and Long-Term Management
Evidence supports a primarily conservative approach for most episodes of lower back pain incurred during simple movements:
Acute Management
- Relative Rest: Brief period (no more than 1–2 days) to avoid aggravating movement,but early mobilization is preferred.
- Heat or Cold Packs: Reduce muscle spasm and pain.
- non-Steroidal Anti-Inflammatory Drugs (NSAIDs): For symptom control if not contraindicated [Mayo Clinic].
- Physical Therapy: Individualized exercise programs optimize recovery, addressing core strength, flexibility, and body mechanics [PMC].
Chronic Management
- Exercise Therapy: Focused on long-term strengthening and flexibility.
- Education and reassurance: Patient engagement and understanding of pain mechanisms reduce fear and promote activity.
- Manual therapy: Judicious use of spinal manipulation or massage when indicated.
- Cognitive Behavioral Therapy (CBT): May help in chronic pain with psychological overlay [JAMA].
- Judicious use of medications: Muscle relaxants or short-term analgesics, with opioids reserved for exceptional cases.
- Surgical interventions: Reserved for severe structural abnormalities or refractory neurologic compromise.
Evidence on Prevention: Practical Strategies
Preventing lower back pain—especially during simple movements—requires a multifactorial approach:
- Regular Physical Activity: Activities that build core and lower back strength, such as walking, swimming, yoga, and Pilates, are beneficial [Harvard Health].
- Optimizing Ergonomics: Adjust workspaces and daily tasks to promote neutral spine alignment. Use supportive seating and correct lifting techniques.
- weight Management: Maintain a healthy weight to reduce lumbar stress [CDC].
- Flexibility Training: Stretch hamstrings, hip flexors, and back muscles regularly.
- ural Awareness: Avoid prolonged static ures; take microbreaks if sitting or standing for long durations.
- Smoking Cessation: Reduces risk of disc degeneration.
- Proper Warm-Up: Before physical activity, warm up and stretch to reduce risk of acute strain.
Living with Lower Back Pain: Quality of Life and Mental Health
Frequent or persistent back pain can impact psychological well-being, leading to anxiety, depression, and social withdrawal. proactive pain management, guided rehabilitation, and mental health support are crucial to restoring function and quality of life [Medical News Today]. Support groups and cognitive strategies can offer additional benefits for coping with chronic pain syndromes.
When to See a Specialist
Referral to an orthopedist, neurologist, physiatrist, or pain management specialist is warranted when:
- Pain persists beyond 6 weeks despite conservative care
- There is importent or progressive neurological deficit
- Structural abnormality is suspected or confirmed
- Pain severely limits daily functioning or occupational performance
- Red flags (see above) are present
A multidisciplinary approach may be necessary in complex or refractory cases [PMC].
Prognosis: What to Expect
Most cases of acute lower back pain resolve within 4–6 weeks with conservative measures. However, recurrence is common unless underlying risk factors are addressed. Chronicity develops in approximately 20% of individuals, among whom pain may persist or recur frequently [NHS]. Adherence to preventive and therapeutic strategies is key to improving long-term outcomes.
Future Directions in Research and Treatment
Emerging research seeks to elucidate the precise mechanisms underlying “idiopathic” back pain—that is, pain during simple movements not explained by current imaging or diagnostic techniques. Advances in motion analysis, neuromuscular assessment, regenerative medicine (e.g., stem cell therapy), and biofeedback-based rehabilitation hold promise [PMC]. Digital health platforms offering tele-rehabilitation, remote guidance, and outcomes tracking are expanding accessibility to high-quality back pain care.
Conclusion
Lower back pain during simple movements you did not expect is a widespread, often distressing phenomenon influenced by diverse mechanical, physiological, and lifestyle factors. While most cases are benign and respond to conservative measures, recognizing risk factors, implementing preventive strategies, and seeking qualified medical evaluation for atypical features is critical. As research continues to evolve, individualized, evidence-based management and proactive self-care offer the best route to recovery and sustained spinal health.
For further authoritative guidance, consult resources from the Mayo Clinic, NHS, and CDC.
References
- World Health Organization: Low back pain factsheet
- CDC: FastStats – Back Pain
- PubMed: Low Back pain Epidemiology
- NIH: Back Pain Information
- Mayo Clinic: Back Pain Causes
- Harvard Health: Facet Joints and Back Pain
- Healthline: Lower Back Pain Overview
- PMC: Physical Therapy in Low Back Pain