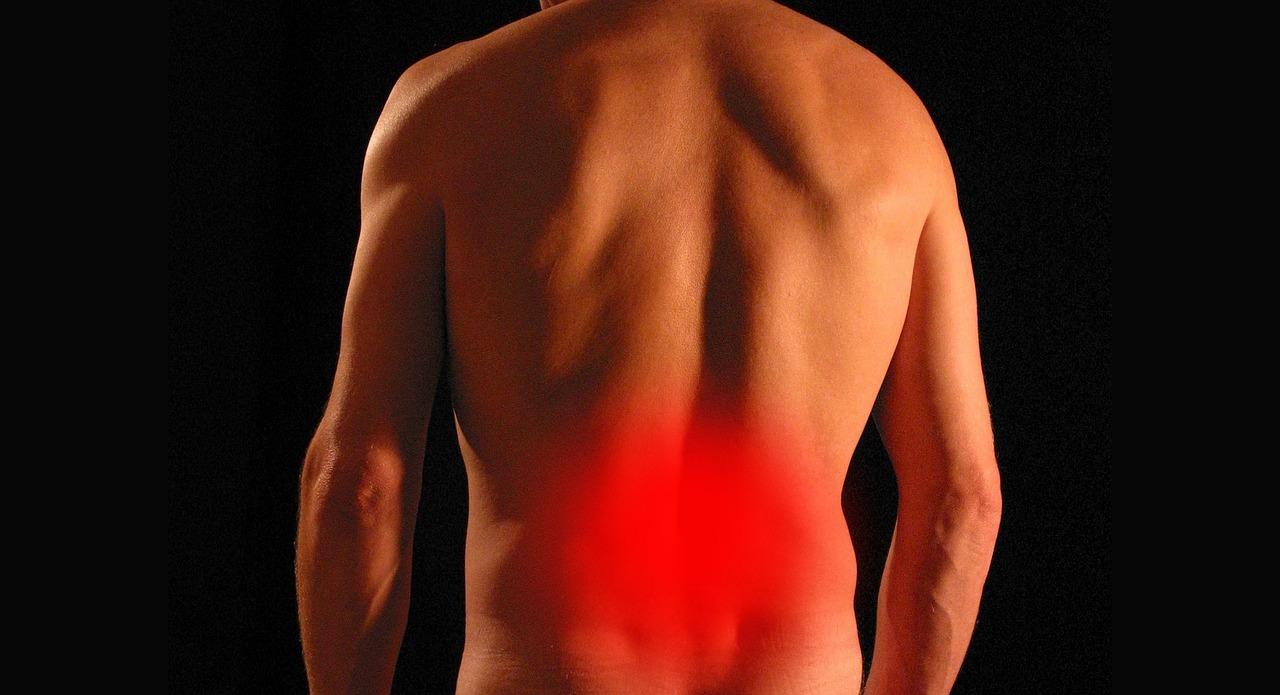
lower back pain and stiffness that make daily tasks tough
Introduction
Lower back pain and stiffness that make daily tasks difficult represent a critically important public health challenge worldwide. Affecting people of all ages,this condition is a leading cause of disability and doctor visits,impacting work,mobility,and overall quality of life. According to the World Health Organization (WHO), musculoskeletal conditions like lower back pain are one of the top contributors to years lived with disability globally. In the United States alone, nearly 25% of adults reported experiencing lower back pain in the past three months. This article explores the clinical, epidemiological, and therapeutic landscape of lower back pain and stiffness, offering evidence-based insights for individuals, caregivers, and healthcare professionals seeking to manage or prevent this pervasive issue.
Overview and Definition
Lower back pain (LBP) is medically defined as discomfort, pain, or stiffness localized to the lumbar region of the spine, typically between the lower rib cage and the gluteal folds. The stiffness component often exacerbates functional limitations, making routine activities such as bending, sitting, or standing challenging. LBP is broadly classified into:
- Acute: Lasting less than six weeks
- Subacute: Lasting six to twelve weeks
- Chronic: lasting more than twelve weeks
The lumbar spine supports much of the body’s weight and is involved in most daily movements, making it notably prone to injury and degeneration. According to the National Institutes of Health (NIH), approximately 60-80% of adults will experience lower back pain at some point in their lives. The high prevalence underscores the importance of early recognition, preventive strategies, and evidence-based management.
Causes and Risk Factors
Multiple biological, environmental, occupational, and psychological factors contribute to lower back pain and stiffness. Understanding these triggers is pivotal for both individualized treatment and public health prevention strategies.
Musculoskeletal and Structural Causes
- Muscle or Ligament Strain: Overexertion, heavy lifting, or abrupt movements can stretch or tear soft tissues supporting the lumbar vertebrae. Such injuries frequently enough lead to acute lower back pain and stiffness, as the body’s inflammatory response generates localized swelling and discomfort (Mayo Clinic).
- Herniated or Bulging Discs: Intervertebral discs act as cushions between the spine’s bones. Disc herniation or degeneration can compress nearby nerves,causing both pain and muscle tightness (Harvard Health).
- Facet Joint Osteoarthritis: Like other joints, the small facet joints can become arthritic, leading to stiffness, decreased adaptability, and referred pain.
Systemic and Inflammatory Conditions
- Ankylosing Spondylitis: A chronic inflammatory arthritis mostly affecting young adults, causing significant stiffness and reduced spinal mobility (NHS UK).
- Other Inflammatory Disorders: Conditions such as rheumatoid arthritis or infections (osteomyelitis, discitis) can increase local inflammation and contribute to rigidity (NIH).
Lifestyle and Occupational Risk Factors
- Poor ure: Prolonged periods of sitting, especially with inadequate back support, are strongly linked to the progress of lumbar stiffness and chronic pain.
- Obesity: Excess body weight increases mechanical strain on spinal structures, accelerating degenerative changes (CDC).
- Repetitive Lifting/Twisting: Occupations that involve frequent heavy lifting or twisting motions can precipitate lumbar muscle injuries and cumulative strain (NIOSH – CDC).
Other Predisposing Factors
- age: Spinal degeneration, including disc wear and bone density loss, is more common with advancing age.
- Genetics: Family history can influence the risk, as certain hereditary spinal abnormalities predispose individuals to musculoskeletal pain (NIH).
- Mental Health: Chronic stress, depression, and anxiety both amplify the perception of pain and can contribute to muscle tension (Harvard Health).
Symptomatology and Clinical Presentation
Patients with lower back pain and stiffness may experience a wide spectrum of symptoms that frequently enough interfere with daily activities. Key features include:
- Pain: Dull ache, sharp shooting pain, or “pins and needles” radiation to the buttocks or legs (sciatica).
- Stiffness: Restricted range of motion, particularly upon waking or after periods of inactivity.
- Muscle Spasms: Sudden and involuntary contractions adding to the overall discomfort.
- Difficulty Performing Tasks: Problems getting up from a chair, lifting objects, dressing, or even walking short distances.
- Associated Neurological Signs: In severe cases, numbness, tingling, or weakness in the legs (indicative of nerve involvement).
Red flag symptoms such as loss of bladder or bowel control, progressive leg weakness, unexplained weight loss, or fever alongside back pain require immediate medical evaluation (Mayo Clinic).
Diagnosis
The diagnostic process for lower back pain and stiffness integrates patient history, physical examination, and selectively, advanced imaging or laboratory studies.
History and Physical Examination
- Clinical History: Duration, severity, progression, precipitating and alleviating factors, previous episodes, occupation, and psychosocial background.
- Physical Exam: Assessment of spinal alignment, local tenderness, nerve root irritation (straight leg raise test), strength, and flexibility.
Imaging
- X-rays: Useful primarily for suspected fractures or advanced degeneration (NHS UK).
- MRI: Indicated when nerve involvement, infection, or malignancy is suspected; provides detailed soft tissue contrast.
- CT Scan: Sometimes used for complex bony anatomy or when MRI is contraindicated.
Laboratory Testing
- Blood tests are usually reserved for evaluation of suspected systemic or infectious causes (e.g.,elevated inflammatory markers in ankylosing spondylitis or infection).
Differential Diagnosis
- Lumbar disc disease
- Myofascial pain syndrome
- Osteoporotic fracture
- Spinal stenosis
- Autoimmune and infectious pathologies
The diagnostic strategy should be individualized, focusing on excluding dangerous underlying conditions and tailoring management (NIH – StatPearls).
Impact on Daily Life
Chronic lower back pain and stiffness profoundly effect individuals’ daily functioning. Evidence suggests:
- Reduced Mobility: Difficulty with walking, climbing stairs, or maintaining prolonged ures (CDC).
- Occupational Impairment: Work absenteeism, reduced productivity, and higher risk of job loss or early retirement (NIH).
- Psychological Morbidity: Increased rates of depression, anxiety, and sleep disturbance in those with persistent pain (Harvard Health).
- Social Participation: limitation in recreation, driving, family, and social engagement, leading to reduced quality of life.
Recognizing these multidimensional effects is essential for comprehensive management and long-term recovery.
Current Therapeutic Protocols
Management of lower back pain and stiffness is multifaceted,combining self-care,pharmacological,physical,interventional,and sometimes surgical interventions — all tailored to individual patient needs and the underlying etiology.
Conservative Management
Physical Therapy and Exercise
- Strengthening and Flexibility Programs: Core stabilization, lumbar strengthening, and stretching reduce stiffness and improve function. Supervised exercise therapy can lower recurrence risk (Cochrane Library).
- Manual Therapy: Techniques such as spinal manipulation and mobilization are beneficial for some subgroups (PubMed).
- Aquatic therapy: Water-based exercise may be preferable for individuals with severe pain or poor mobility (Healthline).
Lifestyle and Ergonomic Counseling
- Adoption of ergonomic workstations, ure correction, and safe lifting techniques is critical, particularly for at-risk occupations.
- Weight reduction in overweight individuals reduces load on the lumbar spine (NIH).
Pharmacologic Treatment
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Frist-line agents for most acute and chronic back pain (NHS UK).
- Analgesics: Acetaminophen/paracetamol may be recommended for mild symptoms, though evidence of benefit is mixed (JAMA).
- Muscle Relaxants: Prescribed for acute spasm-related pain, generally short-term use (Mayo Clinic).
- Topical Agents: NSAID gels, lidocaine, or capsaicin creams for localized relief.
- Opioids: Only for severe pain, short duration, and when other measures fail, given long-term risks (FDA).
Non-pharmacological Approaches
- Heat/Ice Therapy: Short-term use for symptom relief (Medical News Today).
- Yoga and Mind-Body Therapy: Demonstrated benefits for pain perception, flexibility, and psychological well-being (Harvard Health).
- Acupuncture: may offer adjunctive benefit in some chronic low back pain cases (CDC).
Interventional and Surgical Management
- Injections: Epidural corticosteroids or nerve root blocks are considered for radicular pain or severe inflammatory cases supplementing conservative therapy (Mayo Clinic).
- Surgical Options: Reserved for refractory cases with neurological compromise (e.g., lumbar discectomy, spinal fusion), with variable success rates and clear surgical indications (NHS UK).
Psychological and Multidisciplinary Approaches
- Cognitive Behavioral Therapy (CBT): Addresses maladaptive beliefs about pain, stress, and promotes functional restoration (NIH).
- Multidisciplinary Rehabilitation: Coordinated care involving physicians,physical therapists,psychologists,and occupational specialists demonstrates superior outcomes for chronic and disabling back pain (NIH).
Prognosis,Recurrence,and Chronicity
The prognosis for acute lower back pain is generally favorable,with many episodes resolving within weeks. However, recurrence rates are high — up to 70% of individuals experience a repeat episode within a year.Transition to chronicity is influenced by:
- Untreated or undertreated acute pain
- Coexisting depression or anxiety
- Workplace dissatisfaction or economic barriers to care
- Lack of social support and physical inactivity
Early intervention, adherence to evidence-based management, and attention to psychosocial factors are vital for improved long-term outcomes.
Prevention and Self-Management Strategies
Long-term prevention of lower back pain and stiffness is achievable through lifestyle optimization and ergonomics:
- Regular Physical Activity: Engaging in aerobic exercise,strength training,and flexibility routines maintain lumbar spine health (CDC).
- ural Awareness: Adopting correct ures while sitting, standing, and lifting helps prevent undue spinal stress.
- Workplace Modifications: Using adjustable desks,supportive chairs,and appropriate footrests can prevent occupational injuries (NIOSH).
- Weight Control and Nutrition: Maintaining a healthy weight and adequate vitamin D/calcium supports bone and disc health.
- Avoidance of Smoking: Tobacco use is a known risk factor for disc degeneration and chronic pain (NIH).
educational interventions and community resources substantially reduce the societal burden of back pain.
When to Seek Medical Attention
Most cases of lower back pain improve with self-care and time. though, urgent evaluation is warranted if pain is accompanied by:
- Neurological deficits (e.g., foot drop, leg weakness)
- Loss of bladder or bowel control
- Fever or unexplained weight loss
- Significant trauma or suspicion of fracture
- Persistent symptoms beyond six weeks or worsening pain despite standard measures
Timely assessment can help prevent irreversible damage and guide advanced treatment strategies (Mayo Clinic).
Emerging Research and Future Directions
Medical advances continue to refine the understanding and treatment of lower back pain and stiffness. Current areas of interest include:
- Biological Therapies: Use of stem cells or growth factors for disc regeneration (NIH).
- Digital Health: Wearable sensors, telemedicine, and AI-guided rehabilitation interventions (Harvard Health).
- Personalized Rehabilitation: Optimizing treatment pathways based on patient genetics, biomechanics, and psychosocial profile.
Ongoing clinical trials are expected to clarify the risks and benefits of these innovative strategies and may transform future care paradigms.
Conclusion
Lower back pain and stiffness that make daily tasks difficult constitute a major clinical and socioeconomic issue, affecting millions worldwide. Understanding the multifactorial causes, evidence-based diagnostic pathways, and current therapeutic guidelines is critical for effective management. Patients, caregivers, and clinicians are encouraged to adopt a holistic approach encompassing lifestyle modification, early intervention, and, when necessary, multidisciplinary care for optimal outcomes. For more information,visit the CDC’s back pain resources or the NHS back pain guidance.

