introduction
Depression is one of the leading causes of disability worldwide, affecting more than 280 million people of all ages and backgrounds, according to the World Health Organization. While depression can impact anyone, it often manifests differently in men, making early recognition especially challenging. Sociocultural expectations, gender norms, and stigma frequently drive men to conceal emotional distress, which can delay diagnosis and intervention. Evidence shows that men are less likely to seek help for depression, yet they face a disproportionately higher rate of suicide compared to women. Identifying the nuanced and frequently masked manifestations of depression in men is not only a matter of individual health-it is a public health imperative.
understanding Depression: Definition and Clinical Features
Depression, also known as major depressive disorder (MDD), is a complex mood disorder characterized by persistent sadness, loss of interest or pleasure in previously rewarding activities, and a variety of cognitive and somatic symptoms. The Centers for disease Control and Prevention (CDC) describes depression as a medical illness that negatively affects how you feel, think, and act, with symptoms ranging from mild to severe. Clinical symptoms typically include:
- Persistent low or irritable mood
- Anhedonia (loss of interest or pleasure)
- Sleep disturbances (insomnia or hypersomnia)
- Appetite or weight changes
- Fatigue or low energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or making decisions
- Recurrent thoughts of death or suicide
However, as research published in JAMA Psychiatry reveals, men may suppress or misattribute thes symptoms, resulting in atypical presentations and complicating early detection.
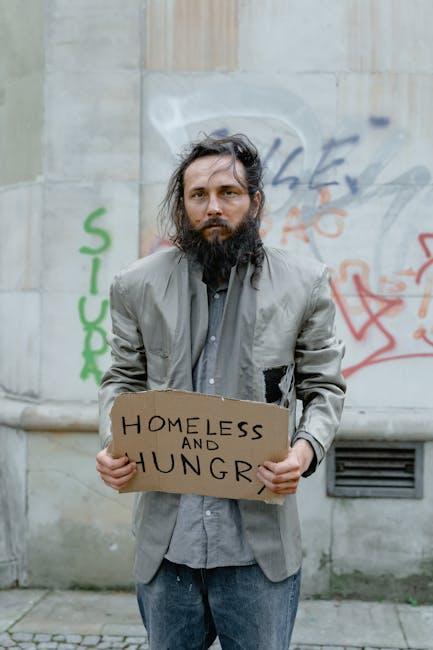
Epidemiology: Depression in Men
The prevalence of depression among men is often underestimated due to underreporting and diagnostic challenges. Data from the National Institute of Mental Health (NIMH) indicate that approximately 6% of adult men in the United States experience major depression each year,yet only a fraction seek professional help. Cultural concepts of masculinity and stoicism can act as barriers to open emotional disclosure,leading to higher rates of undiagnosed and untreated depression and alarmingly higher suicide rates-men account for nearly 80% of all suicides in the U.S., according to the CDC.
Why Do Men hide Depression?
Stigma, Masculinity Norms, and emotional Suppression
Societal expectations play a crucial role in how men experience and express depression. Traditional gender norms often equate masculinity with emotional control, resilience, and self-reliance.Studies reviewed in Harvard Health Publishing highlight that men are conditioned from a young age to associate emotional vulnerability with weakness, leading to the internalization of symptoms or the use of maladaptive coping strategies, such as substance abuse or risk-taking behaviors.
The Journal of MenS Health also reports that stigma associated with mental illness leads men to deny or minimize symptoms, attribute them to external factors (e.g., work stress), or express psychological distress through nonverbal means (e.g., aggression, withdrawal).
Early Signs of Hidden depression in Men
Recognizing concealed depression in men requires a nuanced understanding of its subtle and atypical symptomatology. The following early warning signs are commonly overlooked or misinterpreted. Medical evaluation by a qualified professional is always essential for accurate diagnosis and management.
1. Irritability and Anger
Unlike the classic presentation of persistent sadness, men with depression frequently display increased irritability, frustration, or unexplained anger. Research from The American Journal of Psychiatry indicates that anger attacks and a low tolerance for everyday annoyances are hallmark features of depressive disorders in men, serving as an alternative expression of emotional distress.
2. Physical Symptoms (Somatization)
Men are more likely to report physical complaints-such as headaches, gastrointestinal issues, muscle pain, or chronic fatigue-rather than emotional symptoms. In certain specific cases, these somatic complaints become the primary reason for seeking medical attention, masking the underlying depressive disorder. The Mayo Clinic confirms that unexplained physical symptoms are frequently linked to masked depression, especially in male patients.
3. Changes in Sleep and Appetite
Early shifts in sleep patterns (e.g.,insomnia,hypersomnia) or eating habits (e.g., overeating or appetite loss) often precede the full onset of major depressive episodes. While these signs are common in all forms of depression, studies published in JAMA Psychiatry suggest that men tend to normalize such changes or attribute them to external life circumstances, which delays intervention.
4. Substance Misuse
Alcohol and drug misuse may serve as coping mechanisms for emotional pain that men are unable or unwilling to verbalize. The CDC reports that men with undiagnosed depression are considerably more likely to engage in hazardous drinking or recreational drug use as attempts to self-medicate.
5. Risk-Taking and Compulsive Behaviors
Reckless driving, gambling, extramarital affairs, or compulsive spending are behaviors that may signal an attempt to alleviate feelings of emptiness or numbness associated with depression. Research from Healthline reveals an increased prevalence of impulsivity and risk-taking among depressed men, often as a substitute for traditional symptoms.
6. Social Withdrawal and Isolation
One early yet subtle indicator of male depression is a progressive withdrawal from family, friends, and previously enjoyed activities. What might be perceived as a busy work schedule or desire for solitude can,in fact,represent an effort to distance oneself from social support and scrutiny. Studies in Social Psychiatry and Psychiatric Epidemiology have highlighted the association between social isolation and worsening depressive symptoms in men.
7. decline in Performance at Work or Home
A notable decrease in motivation, productivity, or reliability at work or in domestic responsibilities can be an early manifestation of depression. The National Center for Biotechnology Facts (NCBI) emphasizes that such declines are frequently enough rationalized by men as temporary burnout or external stressors.
8. Difficulty Concentrating or Making Decisions
Cognitive symptoms,such as poor concentration,indecisiveness,or memory lapses,are prevalent but may be dismissed as signs of aging or stress rather than mental health concerns. The Medical News Today resource on depression lists executive dysfunction as a frequent yet overlooked symptom in men.
9. changes in Libido
A diminished interest in sex is both a symptom and a potential result of untreated depression. The Journal of Clinical Psychiatry notes that many men are reluctant to discuss sexual health concerns, instead attributing changes in libido to aging or relationship stress.
10. Persistent Hopelessness or cynicism
Expressions of hopelessness,cynicism,or a negative outlook on the future might potentially be subtle attempts to articulate inner distress. According to harvard Health Publishing, frequent pessimism or fatalistic statements are red flags for further assessment.
Table: Gender Differences in Depression Symptom Presentation
| Symptom Domain | Typical Presentation in Women | Typical Presentation in Men |
|---|---|---|
| Mood | Sadness,tearfulness | Irritability,anger,restlessness |
| Somatic | Fatigue,appetite changes | Headaches,muscle aches,digestive issues |
| Cognition | Guilt,rumination,indecision | Poor concentration,cynicism,risk-taking |
| Behavior | social withdrawal,crying | Substance misuse,reckless behaviors |
| Communication | Seeking support | Minimization,denial,sarcasm |
The Role of comorbidity in Male depression
It is critical to recognize that depression in men frequently co-occurs with other psychiatric or medical conditions.The presence of comorbidities such as anxiety disorders, substance use disorders, or chronic illnesses (e.g.,cardiovascular disease,diabetes) can obscure the primary diagnosis and complicate treatment protocols. For more, see JAMA‘s review on depression and comorbid illness.
Men with coexisting physical or psychological disorders are at increased risk for treatment resistance,functional impairment,and adverse health outcomes. Integrated assessment strategies are crucial for comprehensive care.
Screening Tools for Depression in Men
Because men may underreport emotional distress or deny classic symptoms, validated screening instruments are essential for early detection. Among the widely used tools:
- The Patient Health Questionnaire-9 (PHQ-9) is a brief, self-administered scale widely validated for depression screening (NIH).
- The Beck Depression Inventory (BDI) measures depressive symptom severity (NCBI).
- The Male Depression Risk Scale is tailored specifically for gender-typical symptoms, such as anger and risky behaviors (PubMed).
Screenings should be performed by primary care physicians, mental health professionals, or via workplace wellness programs, supported by confidential follow-up mechanisms.
How to Support men Who May Be Hiding Depression
Communication Strategies
- Open-Ended questions: Facilitating non-judgmental dialogue helps counteract defensiveness.
- Affirmation of Privacy and Safety: Reassure confidentiality to enable emotional sharing.
- Focus on functionality: Asking about day-to-day challenges or performance rather than feelings can elicit more genuine responses (NHS).
Encouraging Help-seeking Behavior
Decreasing stigma and promoting access to supportive resources are proven strategies. Educating men about the physical health impacts of depression,normalizing help-seeking as a strength,and connecting them with peer role models can improve engagement. Public awareness campaigns, such as those led by men’s Health Forum,have successfully reduced barriers.
When to Seek Professional Help
It is vital to seek medical or psychiatric evaluation if early signs of depression persist for more than two weeks, interfere with daily functioning, or are accompanied by suicidal thoughts or risk-taking behavior. Emergency intervention is warranted if there is any indication of self-harm or harm to others (SAMHSA 988 Suicide & Crisis Lifeline).
Barriers to Diagnosis and Treatment in Men
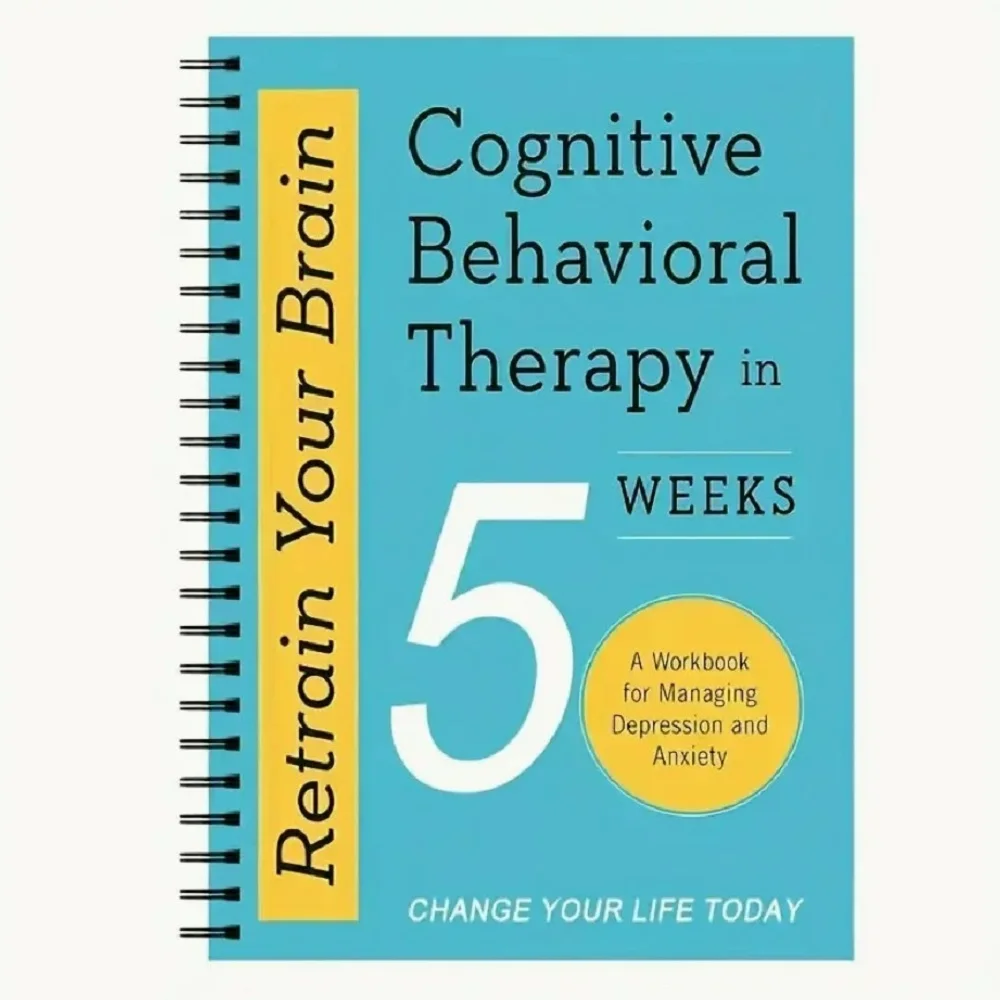
Despite the availability of effective treatments-including cognitive behavioral therapy (CBT), antidepressant medication, and lifestyle interventions-men are less likely to access care. Common barriers include:
- Fear of social stigma or job-related repercussions
- Lack of awareness of depressive symptoms
- Mistrust of mental health systems
- Practical obstacles, such as scheduling or costs (NIH)
Targeted outreach and culturally sensitive education can definitely help close the gap in diagnosis and care.
Therapeutic Interventions: Evidence-based Approaches
Current clinical guidelines recommend a combination of pharmacotherapy, psychotherapy, and lifestyle modification for the management of depression. For men, individualized approaches that address emotional, behavioral, and physical health are most effective (NICE Guidelines).
- Psychotherapy: CBT and interpersonal therapy are first-line options, proven to reduce symptom severity and improve function (NCBI).
- Pharmacotherapy: Selective serotonin reuptake inhibitors (SSRIs) and other antidepressants are commonly prescribed, with adjustments based on patient response and tolerability (Mayo Clinic).
- Lifestyle Modifications: Regular exercise,sleep hygiene,social engagement,and nutritional support can enhance recovery (Healthline).
- Peer and Group support: Peer-led groups and family therapy help counteract isolation and improve outcomes (NIH).
Prognosis: What Is the Outlook for men With hidden depression?
With timely recognition and comprehensive intervention, the prognosis for depression in men is favorable. Untreated depression, however, increases the risk for chronic disease, substance use disorders, relationship breakdown, and suicide. Longitudinal studies in The Lancet demonstrate that early intervention greatly improves quality of life, occupational functioning, and overall health outcomes.
Prevention and Public Health Strategies
Prevention efforts target education, stigma reduction, and increased access to mental health screening. Workplace wellness programs, primary care integration, and public health campaigns can definitely help identify at-risk men and facilitate prompt referrals (NIH). Ongoing research emphasizes the importance of community-based interventions and digital mental health platforms for men reluctant to seek in-person help.
Conclusion
Recognizing the early and frequently enough cloaked signs of depression in men is essential for timely intervention and positive health outcomes.For healthcare providers, family members, and society at large, increasing understanding and reducing stigma are critical steps. By fostering supportive environments, promoting help-seeking, and delivering evidence-based care, we can save lives and enhance wellbeing for millions of men worldwide.
For immediate support, contact your country’s national mental health helpline, or consult a qualified healthcare provider.
References
- world Health Organization: Depression
- CDC: Depression
- NIMH: Major Depression Data
- JAMA psychiatry: Sex differences in depression presentation
- Mayo Clinic: Depression
- Harvard Health: Male depression
- Medical news Today: Depression
- healthline: Depression in Men
- NCBI: Impact of Depression at Work
- SAMHSA: 988 Suicide & Crisis Lifeline
- NHS: Clinical Depression
- Men’s Health Forum
- NIH: Mental health Barriers in Men
- Healthline: Lifestyle and Depression
- NIH: Peer Support Mental Health
- The Lancet: Depression Outcomes
- NIH: Digital Mental Health for Men